The nervous system is an absolute marvel. Most of the time, it works brilliantly, enabling sensation, movement, and a range of other functions like breathing or digesting food.
Nerves exist throughout the entire body. Twelve cranial nerves originate in the brain – and a key one is the trigeminal nerve.
Overview of the trigeminal nerve
The trigeminal nerve is the fifth (CN V) and largest of the 12 pairs of cranial nerves. One trigeminal nerve runs down the left side of the face while the other runs down the right side. The trigeminal nerve’s function is to provide sensation to the face and inside the mouth.
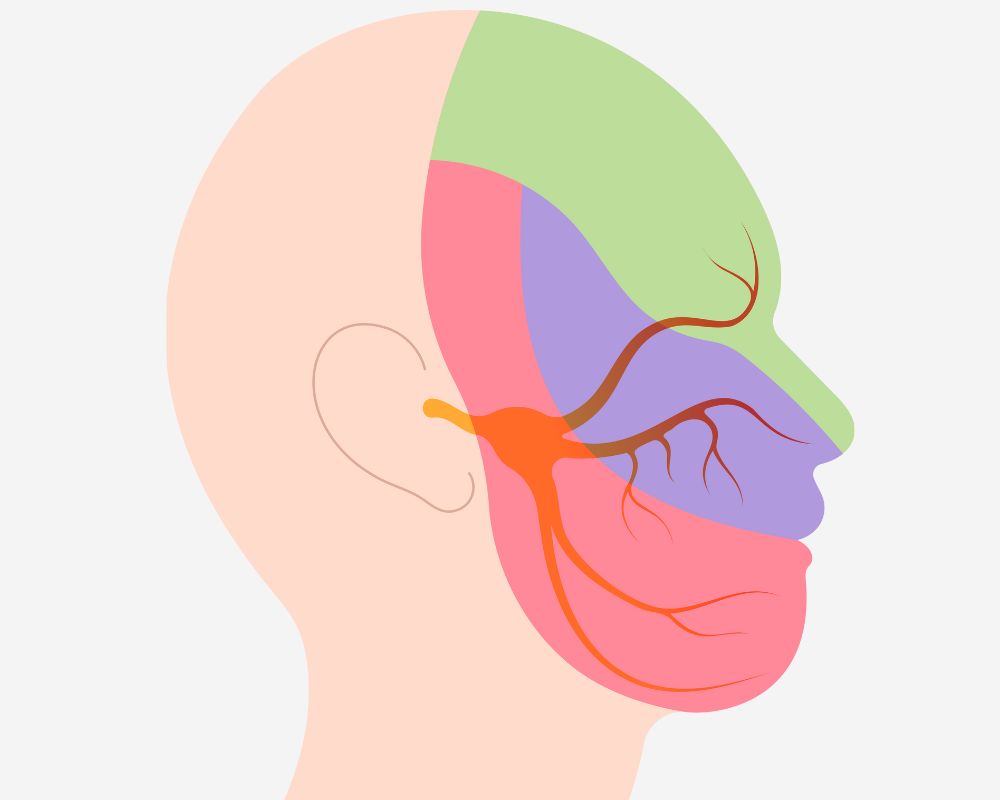
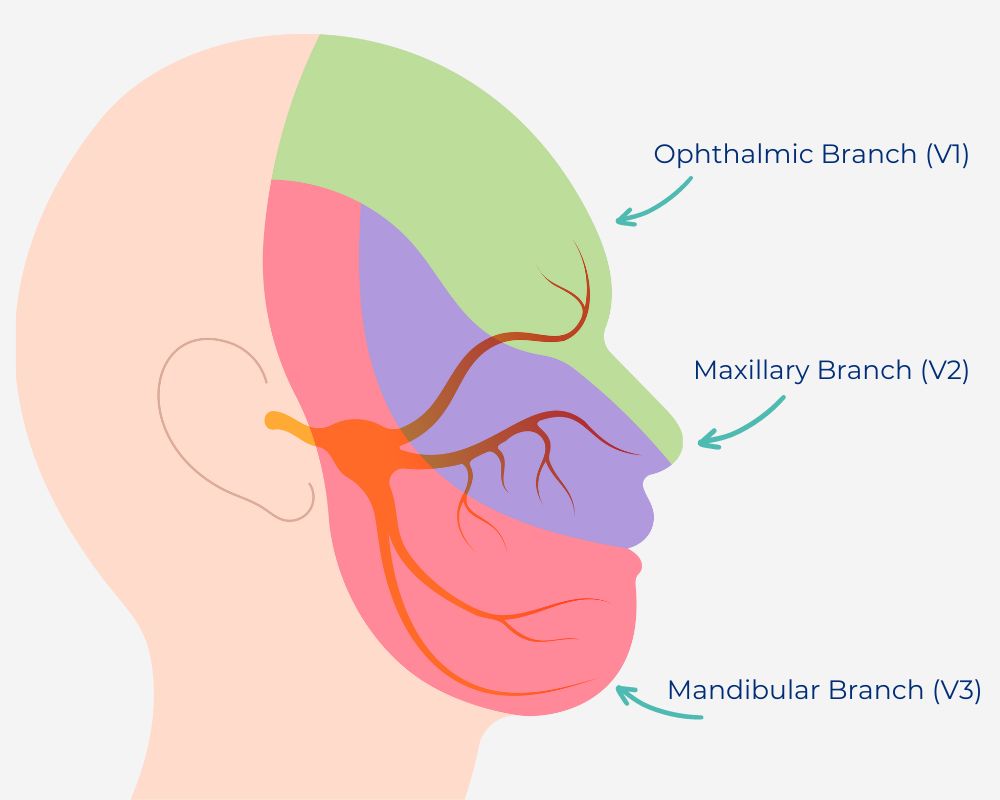
Trigeminal nerve branches
The trigeminal ganglion sits on the base of the skull just in front of the ear and behind the eye. From that point, the trigeminal nerve divides into three branches that supply the upper, middle, and lower parts of the face.
Ophthalmic branch (V1)
The ophthalmic (eye) branch of the trigeminal nerve enables sensation and movement in the eyes, upper eyelids and forehead.
Maxillary branch (V2)
The maxillary (upper jaw) branch provides sensation to the middle part of the face. This nerve extends to the cheeks, nose, lower eyelids, upper lips and gums.
Mandibular branch (V3)
The mandibular (lower jaw) branch supports sensation to the lower part of the face such as the jaws, lower lip and gums. Separately a motor branch travels with this that enables biting, chewing, and swallowing.
Trigeminal neuralgia
Trigeminal neuralgia is a condition involving pain on one side of the face. There are three key types.
Classical trigeminal neuralgia
Classical trigeminal neuralgia can be diagnosed when:
- A patient experiences repeated attacks of one-sided facial pain
- There is evidence of an artery or vein compressing the nerve together with changes in the trigeminal nerve root itself (these may be detected on MRI or in surgery).
Many patients with classical trigeminal neuralgia can clearly remember when the pain began. There may be pain-free periods followed by a sudden recurrence of pain. In some patients, the pain is constant and does not go away.
Secondary trigeminal neuralgia
In this type, neuralgia occurs as a result of another underlying condition.
Patients may have:
- Persistent or recurrent one-sided facial pain
- An underlying condition such as:
- Multiple sclerosis
- Arteriovenous (AV) malformation – when the nerves and veins are abnormally tangled
- A tumour
- Damage caused by surgery.
Secondary trigeminal neuralgia may be diagnosed when that combination of factors exists and there is no other plausible explanation for the pain.
MRI may be useful in identifying the underlying condition. Doctors may also assess trigeminal reflexes.
Idiopathic trigeminal neuralgia
‘Idiopathic’ means a condition without a known cause.
Idiopathic trigeminal neuralgia may be diagnosed when:
- A patient experiences persistent or recurrent one-sided facial pain that meets the definition of trigeminal neuralgia
- Investigations have ruled out classical trigeminal neuralgia and secondary trigeminal neuralgia
- No other diagnosis fits the pattern of symptoms.
Diagnosing trigeminal neuralgia
Trigeminal neuralgia can be difficult to diagnose because there is no specific test to assess the health of the nerve.
Many conditions cause similar symptoms to trigeminal neuralgia. They can include:
- Sinus infections
- Cluster headaches
- Trigeminal neuropathic pain
- Temporomandibular joint syndrome
- Dental pain.
Patients are encouraged to seek medical care when experiencing facial pain, especially when they have not had recent dental or facial surgery. Healthcare professionals are encouraged to consider trigeminal nerve involvement in patients presenting with facial pain.
Diagnosing trigeminal neuralgia may involve:
- Obtaining a detailed medical history of how the pain feels, where it is located and what triggers it.
- An MRI scan to find out if anything is affecting the nerve
- A physical and neurological examination to explore the location of the pain
Treatments for trigeminal neuralgia
Treatment focuses on relieving pain and may include:
- Medications – several options are available, generally starting with low doses anti-epileptic drugs. (carbamazepine)
- Percutaneous procedures – these damage the nerve to reduce abnormal transmissions of sensation that cause the pain. Examples balloon compression, radiofrequency ablation.
- Radiosurgery – focused beam of radiotherapy performed in one setting. Which damages the nerve and reduces abnormal transmissions.
- Surgery – (Microvascular decompression) to remove or separate the offending artery or vein from the nerve.
It is important to remember that all treatments involve a trade-off between benefits and risks. These are important areas for discussion between patients and doctors.
Next steps
If you are a patient experiencing facial pain, please talk to your GP in the first instance. They may examine you, order tests or refer you to a neurologist or neurosurgeon if necessary. If you would like to see one of our specialists and already have a referral, please book an appointment.
If you are a doctor keen to advance your knowledge of neurosurgery, please sign up for one of our workshops.
Disclaimer
All information is general and is not intended to be a substitute for professional medical advice. Macquarie Neurosurgery and Spine can consult with you to confirm if a particular treatment or procedure is right for you. Any surgical or invasive procedure carries risks. A second opinion may help you decide if a particular treatment is right for you.
References
- Huff T, Weisbrod LJ, Daly DT. Neuroanatomy, Cranial Nerve 5 (Trigeminal) [Updated 2022 Nov 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482283/, [Accessed 11 January 2024]
- Cleveland Clinic, Trigeminal nerve, https://my.clevelandclinic.org/health/body/21581-trigeminal-nerve, [Accessed 11 January 2024]
- Cleveland Clinic, Trigeminal neuralgia, https://my.clevelandclinic.org/health/diseases/15671-trigeminal-neuralgia-tn, [Accessed 11 January 2024]
- Multiple Sclerosis Trust, Trigeminal neuralgia, https://mstrust.org.uk/a-z/trigeminal-neuralgia#, [Accessed 11 January 2024]
- American Association of Neurological Surgeons, Trigeminal neuralgia, https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Trigeminal-Neuralgia, [Accessed 11 January 2024]