Non-Instrumented Spine Surgery

Non-instrumented spine surgery is surgery to treat spinal problems without the need to include implants.
Most commonly, implants are included for fusion surgery, but non fusion implants are occasionally used.
Non-instrumented spinal procedures are most commonly done in order to relieve pain from irritation or compression of the nerve roots in or as they leave the spinal canal. Less commonly the spinal cord itself is compressed and requires decompression.
There are a variety of different problems than can affect the spine, the most common ones are degenerative conditions, and disc herniations.
Examples Of Non-Instrumented Spinal Procedures
- Lumbar laminectomy
- Lumbar microdiscectomy
- Thoracic laminectomy
- Thoracic discectomy
- Posterior cervical foraminotomy
- Posterior cervical laminectomy

Indications For Surgical Decompression Of The Spine
Before deciding on any spinal procedure, the patient’s general health, severity of symptoms as well as their effects on their quality of life, are all very important factors to consider.
Lumbar laminectomy may be an option if the patient has lumbar degenerative disease and/or disc herniation causing narrowing of your spinal canal, or foramen. Foramina are the passages in the vertebrae through which the nerves come out of the spinal canal. The nerves are commonly affected by degenerative processes in the foramina. This usually causes a range of pain symptoms where the patient’s leg(s) will often be affected to a greater degree than their back.
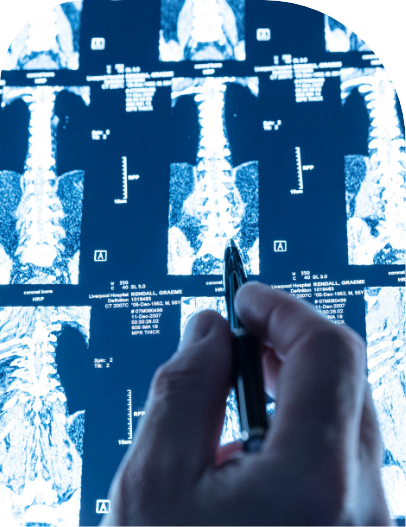
Stenosis is the medical term used to describe narrowing of the spine elements which can cause symptoms.
Investigations such as CT or MRI will often use this term in the report on the spinal level where surgery is being suggested.
Examples of typical presentation:
- Leg pain or weakness that is disabling and limits activities, especially walking
- Weakness and sensory changes of the leg(s) and feet
- Leg pain which worsens while walking a certain distance and gets better after a short period of sitting down, leaning forward, or lying down
There may or not be back pain associated with the leg pain.
Other Treatment Options
There are many alternatives to surgical options for treatment of degenerative spinal stenosis:
- Pain medication
- Steroid injections: perineurial, epidural image guided cortisone injections aim to reduce inflammation which causes pain
- Physiotherapy helps improve function and muscular support of the spine
- Patients may also choose to not do anything special, simply allowing time and natural healing to settle inflammation
All the above are good options and depending on the level of symptoms, the patient’s imaging and examination findings, their GP or pain specialist will be able to guide them through the process.
It is however important to note that there are a few rare conditions that can require urgent consultation, such as severe weakness of legs or feet, difficulty with bowel and bladder control especially if associated with numbness in the saddle areas, i.e., around the genitalia or the back passage. In this rare event urgent neurosurgical consultation is advised.
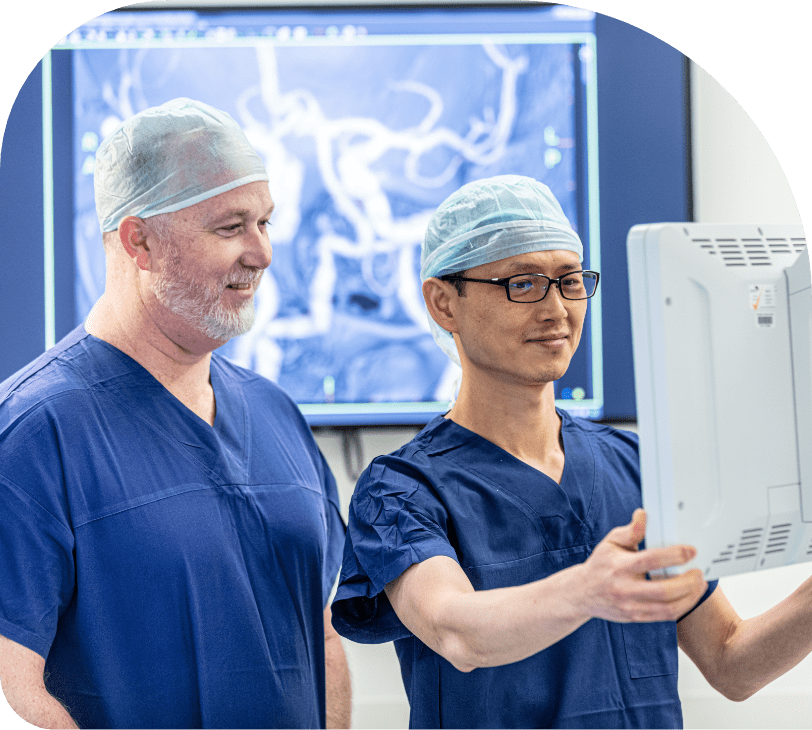
Procedure Details
Laminectomy (removal of part or whole of the lamina to decompress the nerves), Microdiscectomy (removal of a disc prolapse causing pressure on a nerve) or foraminotomy (enlarging the foramen to decompress a nerve) are common surgical operations to relieve compression on nerves or spinal cord caused by degenerative processes.
The main objective of the procedure is to remove pressure by widening the lumbar spinal canal through an incision in the back.
The operation is typically performed on a patient under general anesthesia, positioned on a special operating table, with the patient lying face down to expose the lower back.
With the help of intra-operative x-rays, a small incision is made directly on the level(s) which need decompression, then the bony posterior aspects of the surgical levels of interest, namely the spinous processes and laminae are exposed.
Decompression consists of removal of parts of the lamina, ligaments and other tissues compressing the nerves or spinal cord at the level of compression.
At the level of the lumbar spine, degenerative process can lead to compression of the nerve roots in their individual nerve channels; the neuroforamina.
The aim of decompression is to make sure these nerve roots are completely free from any compressive effects of ligaments and bone spurs. Hence, decompression at the lumbar spine is often carried laterally into the neuroforamen in a procedure called foraminotomy.
At the level of the cervical spine, when there is narrowing for the nerve channel by degenerative process or herniated disc material, a similar procedure can be done. This consist of carefully removing small portion of bone and spinal joints overlying the nerve root. Herniated disc fragments can also be extracted in the same approach.
In case of intervertebral disc herniation into the spinal canal, lateral recess or neuroforamen, the herniated fragments are carefully identified using microsurgical techniques and removed.
The aim here is not to remove the entire disc. It is mainly to remove the disc herniated fragments to relieve compression of nerve roots which causes inflammation and pain.
There are many other types of less common spinal conditions that can be treated without the need to perform fixation of the spine. These include:
- Spinal tumors
- Spinal vascular malformations
- Spinal CSF leaks.
After The Surgery
Immediately after the operation, every effort will be directed at ensuring the patient’s safety and comfort making sure that their heart and lungs are working normally, and they are comfortable. Patients will typically waken either in the recovery area or intensive care unit. A staff member will attend to each patient to assess their general health, their wound, and check their neurological function regularly in the initial few hours.
After this the patient will be moved to their room when everything is stable. It can be expected to have some discomfort especially at the surgical site and the measures to minimize pain and maximize patient’s comfort will have been discussed with the anesthetist, and nurses will be there to help.
A physical therapist will attend to the patient as soon as advised by their surgeon and the patient will start some physical exercises including walking as tolerated.
Walking early is good for the lungs and helps prevent the risk of blood clots (DVT) forming in the legs and accelerates recovery.
Medications After Surgery:
- Patient will receive at least 3 doses of antibiotics
- Patient will receive pain medications as directed by pain specialist team
- Unless otherwise advised, patient will also receive anticoagulation medications to prevent DVTs
- Some of their regular medications will also be resumed/continued if they have no adverse effects vis a vis the surgery.
Most patients are discharged two to three days after surgery.
Possible Complication Of Spinal Decompression Procedures
Although spinal decompression procedures are known to be tremendously effective in selected patients, they can be associated with serious complications like any other surgical procedures:
The complication can be divided into general risk of surgical procedure and specific early and late complications associated with the procedure performed:
Common
- Surgical site infection or bleeding
Less common
- Excessive bleeding during the operation requiring a blood transfusion post operatively
Less common but serious
- Blood clots in the legs (DVT) or in the lungs (PE)
Rare but extremely serious
- Complications related to anesthesia e.g., Myocardial infarction (heart attack) are very rare but extremely serious or even fatal. Blindness is another extremely rare risk.
- Blood clots in the spinal canal with continued compression of the nerves requiring reoperation for removal of blood clots drainage
- Failure to improve or worsening of symptoms
- Nerve root injury resulting in worsening of leg pain or weakness or sensory impairment or loss
- Spinal cord injury causing transient or permanent paralysis is fortunately very rare but can occur in any spinal procedure
- Recurrence of disc herniation may occur in hospital or months or even years later
- Cerebrospinal fluid leakage due to a tear in the coverings of your neural element (Dural tear) during surgery. This is usually repaired or managed without further complications.
- Increased back pain after surgery requiring more complex surgery
- Abnormal scarring around the nerve can cause delayed recurrence of leg pain due to restricted free movement of the nerve.
- Cosmetic discomfort due to abnormal scarring of skin incision (keloid or hypertrophic scar).
Recommendations For Recovery At Home
Recovery usually takes 3 to 4 weeks after uncomplicated lumbar laminectomy and other types of non-instrumented spine procedures. It may take longer in older patients and in case of severe pre-existing disability.
General Recommendations During This Time
- Avoid lifting heavy objects (more than 2kg).
- Bending and twisting movements should be minimized.
- Get advice from a physiotherapist on how to lift if needed.
- Driving is also usually not allowed for several weeks during recovery.
- Swimming and baths when the wound is dry.
- Stay active: It is recommended to take regular walks and do daily light exercises to relieve back pain and hasten recovery. Sitting for long periods put the operated site at increased pressure.
- Take adequate rest: a good sleep helps the body to recovery faster. Patients may find their back is sore upon waking up, this usually settles after a short walk or a shower.