Tethered Cord Syndrome
Tethered Cord Syndrome is a condition where the spinal cord is abnormally attached to tissues in the spinal canal, restricting its movement and causing damage from stretching.
Tethered Cord Syndrome is a structural and often congenital abnormality at birth but can also be acquired and develop later in life, for example after an injury, bleeding, infection or a tumour.
What are the common symptoms?
Presenting symptoms may vary dependent on age, exact location and extent of tethering, as well as dynamic changes over time like further growth in babies and young children and underlying pathology.
Common symptoms and findings include back pain, pain or weakness in the legs, sensory deficits, bowel and bladder dysfunction and spinal deformities, including scoliosis and Chiari malformation.
Babies may present with foot deformities, and/or an abnormal skin finding on their back including a sacral simple, deviated gluteal crease, midline haemangioma, hair tuft or a subcutaneous lump. Toddlers may present with predominant toe walking, muscular atrophy and lower extremity length discrepancies. Other spinal deformities may also be present.
How is it diagnosed and treated?
Sometimes, a tethered cord is diagnosed incidentally, and patients may be asymptomatic. Nevertheless, in babies and young children prophylactic surgery may be indicated to prevent future neurological deficits with further spine growth and increase in tethering and stretching of the spinal cord.
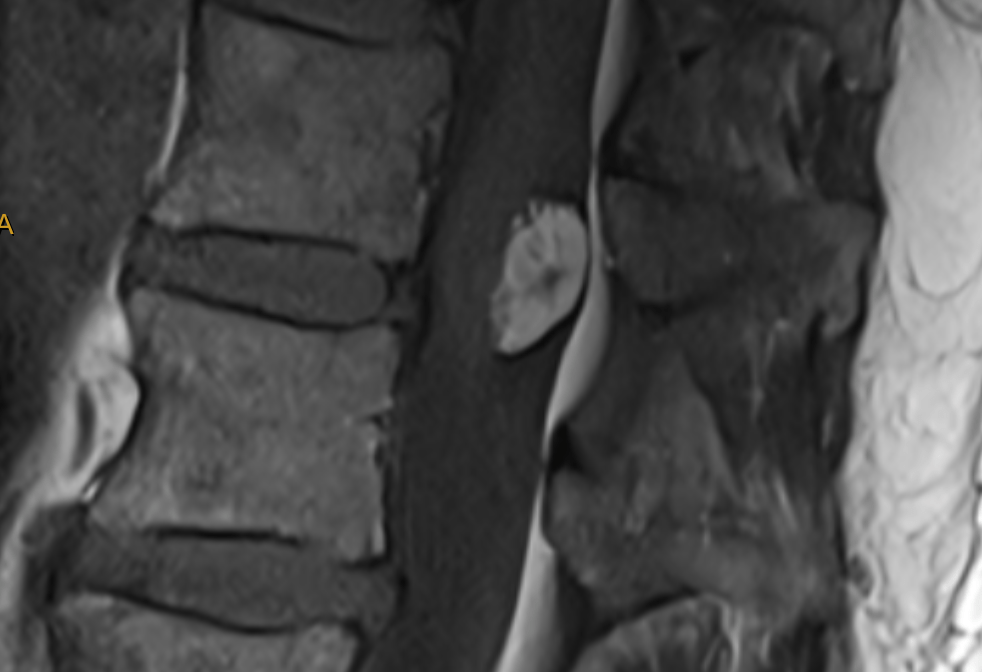
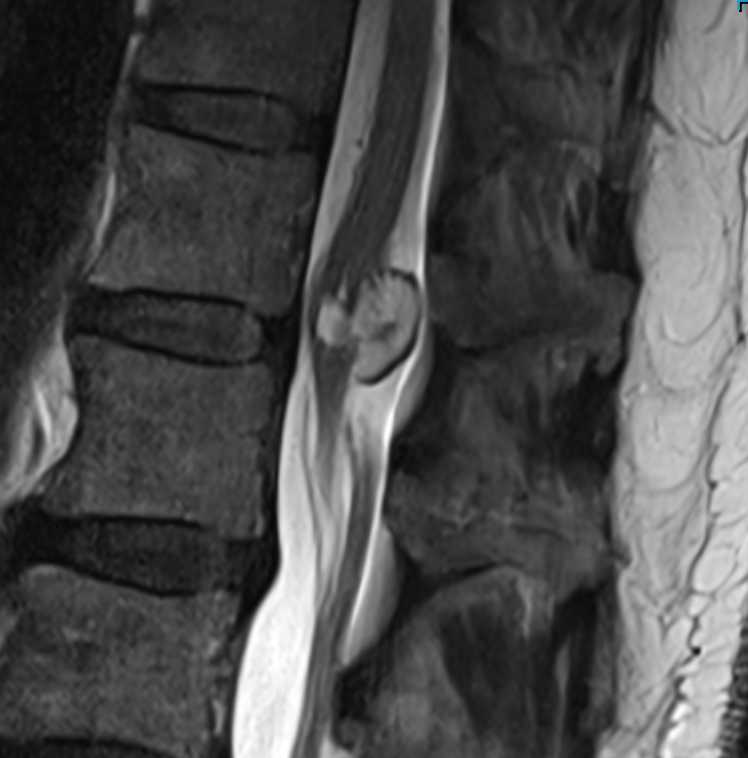
Diagnosis is typically made using MRI, which may require a general anaesthetic in younger children. Treatment depends on the underlying pathology but often involves surgery to release the spinal cord and prevent further spinal cord and nerve damage
Spinal Cord Lipomas
Spinal Cord Lipomas are an example of congenital (from birth) lesions causing tethered cord syndrome.
There are different types of spinal cord lipomas including dorsal lipomas, transitional lipomas and chaotic lipomas. Their classification depends on location and embryological development and also has prognostic value.
Often, but not always they present with a subcutaneous fatty lump on the back. Sometimes suspicious skin findings on the back are more subtle or even absent and may include a dimple, deviated gluteal crease, hair tuft, midline haemangioma or pigmentation deficits. Frequently, lipomas are also associated with other congenital malformations.
Another type of lipoma is the so-called fatty filum which involves an embryological remnant string of tissue just below the spinal cord and is also a tethering lesion.
All different types of lipomas may be discovered incidentally or already present with any of the symptoms of tethered cord syndrome as described above or a combination of them.
Prophylactic surgery is indicated to prevent future neurological deficits with further spine growth and increase in tethering and stretching of the spinal cord.
Diagnosis is typically made with MRI, which may require a general anaesthetic in younger children and babies.
Gold standard treatment involves surgery with complete/total resection of the lipoma if possible and release of the spinal cord to prevent further spinal cord and nerve damage. The surgery is performed under intraoperative neuromonitoring to minimise perioperative risks and enhance surgical safety.
What happens in Tethered Cord Syndrome?
- The spinal cord is normally loose and free
- In Tethered Cord, tissue attachments fix the spinal cord and prevent tension-free movement
- This causes the spinal cord to be stretched and damaged, also limiting adequate blood flow and oxygen perfusion
- This condition can be congenital (from birth) or acquired (due to injury, surgery, or other spinal defects)
Signs and Symptoms
Symptoms can vary and often worsen over time.
- Musculoskeletal: Back pain, leg pain, foot deformities (e.g., high arches, curled toes), weakness or numbness in the legs, scoliosis (abnormal spine curve).
- Neurological: Tremors or spasms in the legs, difficulty walking.
- Urological/Gastrointestinal: Loss of bowel or bladder control, repeated bladder infections.
- Skin findings (in some cases): A fatty mass, hair patch, dimple, or birthmark on the lower back may indicate an underlying defect.
Diagnosis and treatment
- Diagnosis: An MRI is used to image the spinal cord and surrounding structures, confirming the diagnosis and the extent of the tethering.
- Treatment: Surgical release of the tethered cord is the primary treatment to relieve tension and prevent further nerve damage.
Why is treatment important?
- Early diagnosis and treatment can prevent permanent spinal cord/nerve damage and neurological deficits.
- Surgery can improve or halt the progression of neurological, musculoskeletal, and other symptoms.
