Paediatric Chiari Malformation

Patients with Chiari malformation require management by an experienced neurosurgical team. Specialists at Macquarie Neurosurgery & Spine are some of Australia’s leading experts on this condition and its complications.
What is Chiari malformation?
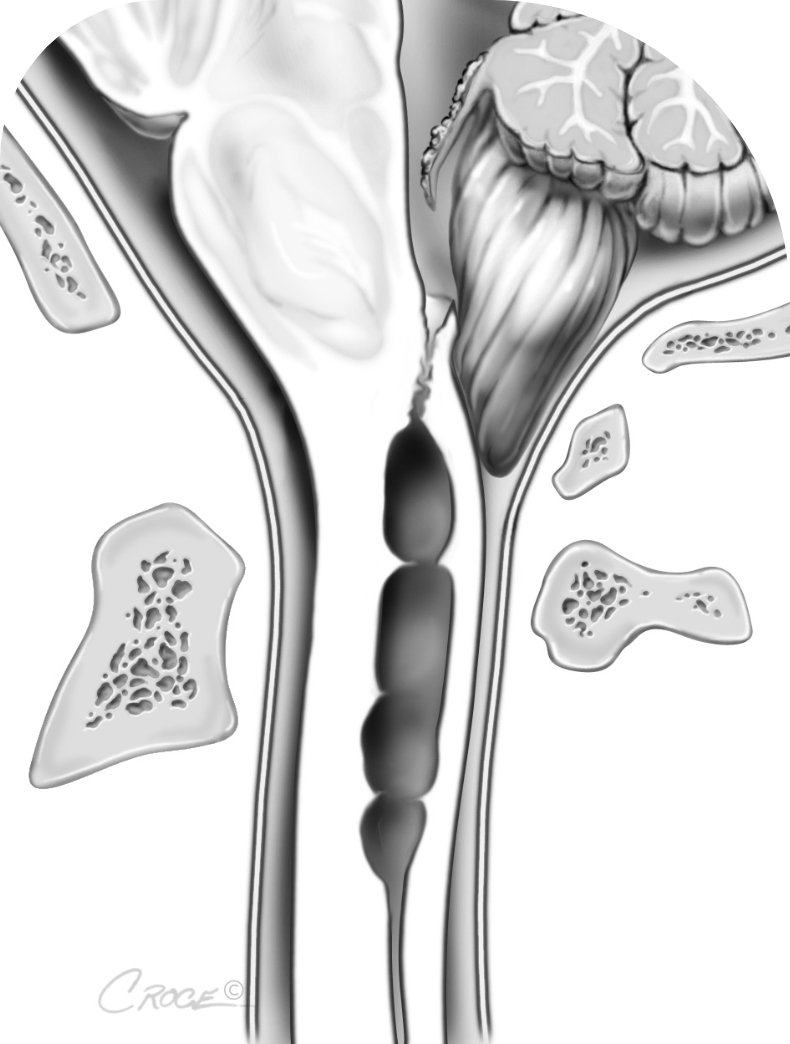
Chiari malformation is a structural and often congenital abnormality that forms already during foetal development. The cerebellum is the back part of your brain, and it coordinates balance and movement. Normally, the cerebellum is found within your skull. In patients with Chiari malformation, part of the cerebellum is squeezed out into the upper spinal canal.
Chiari malformation can block the normal flow of cerebrospinal fluid (CSF) between the brain and spinal cord, causing increased pressure on these structures.
There are different types of this condition. People with Chiari malformation type I may or may not experience symptoms. Type I is the most common Chiari malformation. Other types include type II Chiari malformation (historically known as Arnold-Chiari malformation), which is associated with open myelomeningocele (a type of spina bifida). There are also types III and IV, as well as type 0 and 1.5.
What are the symptoms of Chiari malformation?
Not all patients with Chiari malformation develop symptoms. Quite frequently, the condition is found incidentally when brain imaging is done for other reasons.
Typical symptoms may include occipital headaches and/or neck pain often made worse by straining, sneezing, or coughing. Other symptoms may include loss of coordination, dysbalance, visual disturbances, sleep apnoea, dysphagia.
Secondary, as a result of Chiari malformation some patients may also develop scoliosis, torticollis, hydrocephalus or syringomyelia. Syringomyelia is the formation of cysts in the spinal cord, which itself can cause a wide range of symptoms, but typically leads to muscle weakness, sensory deficits including hypersensitivity in the upper body, arms, and hands.
How is it diagnosed?
Chiari malformation may be diagnosed during investigations for above mentioned symptoms or incidentally when the patient is being tested for other conditions. In some instances, diagnosis is already made on prenatal ultrasound before birth.
Advanced imaging tests enable us to diagnose Chiari malformation and often determine its cause. Magnetic resonance imaging (MRI) produces detailed images of the brain. Both conventional and phase contrast MRI sequences can be used to assess the degree of hindbrain migration. A computerised tomography (CT) scan may also be used, especially to screen for any associated bony abnormalities. At Macquarie University, we use advanced imaging such as dynamic MRI to gain a better understanding of the severity of a Chiari malformation and to guide treatment.
How is Chiari malformation treated?
Treatment of Chiari malformation (and associated syringomyelia) is dependent on age, the type of malformation, degree of herniation and its symptoms.
If the malformation is not causing any symptoms, and has not led to syringomyelia, treatment may not be necessary. If there are severe symptoms, surgery may be considered to relieve pressure on the spinal cord and lower part of the brain, and to restore normal CSF flow.
Different surgical treatment options exist and may vary for different patients, age groups, pathologies and types of Chiari malformation. A so-called suboccipital decompression involves removing a small part of the occipital bone of the skull to create more space for the cerebellum and CSF. In some case, also the back part of the first few neck vertebrae has to be removed (Laminectomy) to create sufficient space. While a bone-only decompression may be sufficient for some patients, in others also the dura is opened and an expansile dural graft be used to provide enough decompression and re-establish CSF flow. Further additional surgical features may be recommended including a 4th ventricular shunt.
Please contact us if you require any further information or for booking a consultation with A/Prof Eibach via admin@mqneurosurgery.com or 02 9812 3900
