Instrumented spine surgery
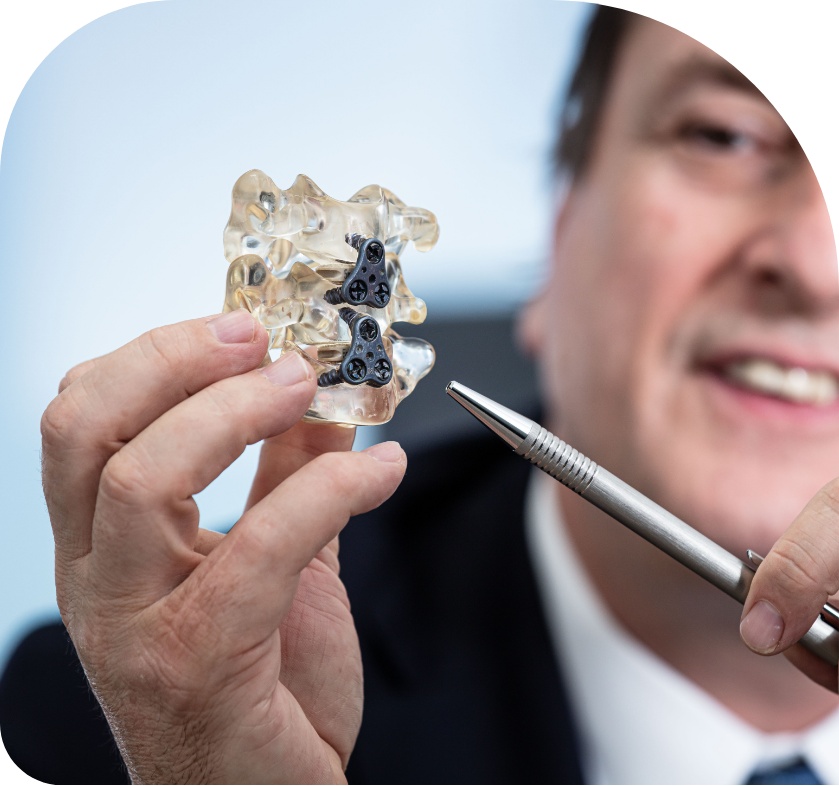
Instrumented spine surgery is surgery performed to treat spinal problems with the use of spinal implants (excluding pain modulation devices).
Instrumented spine surgery can be divided into 2 major categories: Fusion and non-fusion procedures.
Spinal traumatic injuries and degenerative diseases are the most common conditions which might require addition of implants during surgery but a variety of congenital and acquired conditions affecting the spine may also require instrumentation as part of their treatment.
A spine motion segments is defined as two bony levels with an intermediate disc which allows healthy motion to occur. The spinal discs are named after the bones that sit above and below the respective disc. For instance, L4 L5 disc is attached between L4 and L5 vertebral bodies.
Examples of instrumented spine procedures
These are surgical procedures which may include decompression of neural elements but which also include insertion of instrumentation aimed at limiting or eliminating motion at a spinal segment to maximize likelihood of bone healing between motion segments. This may be required to correct the shape of the spine and/or eliminate actual or potentially painful spinal segment motion.
Examples of fusion procedures include:
- Cervical spine:
- Cranio-Cervical fixation.
- Anterior cervical decompression and fixation
- Posterior cervical fixation
- Thoracic and Lumbar spine
- Screws and rods-based fixation procedures in the posterior approach with or without postero-lateral bone grafting
- Inter-body cages are inserted to replace the intervertebral disc by one of many routes either anterior, lateral, oblique, or posterior approaches.
A combination of more than one of the above-mentioned procedures is often selected to obtain optimal fusion and to ensure the spine is fused in the correct shape, which helps to minimize the risk of future problems in the spine.
Indications
The following are some of the more common reasons the surgeon may recommend a fusion procedure to treat a patient’s spinal problems:
- Cervical spine
- Degenerative conditions of the cervical discs and/or facet joints requiring removal of the whole disc to access a disc protrusion or remove bony spurs pressing on the spinal cord or spinal nerves
- Traumatic injuries causing instability (too much movement) at a cervical segment
- Correction of abnormal shape of the spine causing symptoms
- Other conditions where the treatment might cause abnormal motion causing pain or neurological injury.
- Thoracic and lumbar spine
- Degenerative conditions are by far the most common to require a fusion procedure at the lumbar spine, where spine traumatic injury mainly affects thoracic and thoracolumbar junction.
Other less common indications include spinal infections and spine tumours. Spinal deformity (abnormal shape of the spine) conditions may also require fusion procedures
These are specific procedures which avoid fusion and aim to maintain spinal segment motion done by means of special spinal implants aimed at preserving motion.
The commonest example is total disc replacement in the cervical and lumbar spine, where prosthetics are inserted through an anterior (from the front) approach to the spine.
Motion preservation spinal instrumentation is a well-established means of treating a variety of spine conditions including degenerative disc disease. However, the indications are still limited and tend to be suitable for only a minority of surgical patients, and rarely for patients with many levels of degenerative disease.
Procedure details
There are many ways to achieve instrumentation of the spine. For simplicity, we will divide these into anterior and posterior procedures depending on the nature of the approach to the spine and the type of instrumentation achieved; i.e. posterior screws and rod fixation or inter body cage insertion or a combination of both.
Posterior spinal instrumentation procedure
Following standard preparation for major spinal procedures including general anesthesia, the patient is carefully positioned face down on the operating table to expose their back.
Posterior spinal instrumentation can be done on any segment of the spine from occiput to sacral segments (= head to tail). Fluoroscopy or image guidance is often used throughout to ensure accuracy of implantation.
Under sterile conditions, an incision is made on the level of disease to expose its posterior elements. For example, if the surgery is for fusion of lumbar level 4 to Lumbar level 5, all the bony posterior aspects of this motion segment are exposed.
Then screws are inserted in level 4 and level 5 on both sides. A fusion cage between the two vertebral bodies to be fused may be inserted in the same posterior approach or in a different approach discussed in the next section. This cage usually is filled with graft material to promote fusion (bone healing) between both levels. Image guidance is helpful to ensure optimal implant placement.
A rod in fixed into the screws on either side, to link the motion or motion segments, and give it more strength while fusion is taking place.
Modern spine surgery may also incorporate minimally invasive techniques to minimize skin incisions and underlying tissue damage while achieving the same surgical goals
Anterior or lateral spinal instrumentation
Anterior spinal instrumentation is usually performed on cervical and lumbar segments, rarely on thoracic level.
At the lumbar segment, anterior approaches to the spine for fusion are becoming increasingly popular as they help restore the correct shape to the spine.
The aim of this surgery is to achieve fusion of the motion segment from an anterior, oblique or even lateral approach by inserting a fusion cage between the vertebral bodies in a minimally invasive fashion.
More often anterior surgery is combined with a posterior approach to achieve optimal fusion. This can be achieved in a single procedure or in a staged fashion.
What to expect following a spinal fusion procedure?
Immediately after your operation, some discomfort can be expected especially at the surgical site.
Every effort will be directed at ensuring the patient’s comfort.
Patient will typically wake up either in intensive care unit or other highly monitored area (post anesthesia recovery area). A staff member will attend to assess the patient’s general health, vital signs, wound dressing and check their neurological function regularly in the initial few hours to ensure the recovery from anesthesia is smooth.
A physical therapist will attend to the patient as soon as advised by the surgeon and the patient will start some physical exercises including walking as tolerated.
Walking early is good for the lungs, circulation and helps prevent the risk of blood clots (Deep Vein Thrombosis- DVT) forming in the legs, hence accelerates recovery.
Medications after surgery:
- Patient will typically receive at least 3 doses of antibiotics.
- Patient will receive pain medications as directed by our specialized pain team.
- Unless otherwise advised, patient will also receive anticoagulation medications to prevent DVT.
- Some of the patient’s regular medications will also be resumed or continued if they have no adverse effects vis a vis the surgery.
Most patients after fusions spend one or two days in a high/intensive care unit before return to regular ward where they spend 3 to 5 days before going home. This depends of course on the complexity of the surgery and individual recovery pattern.
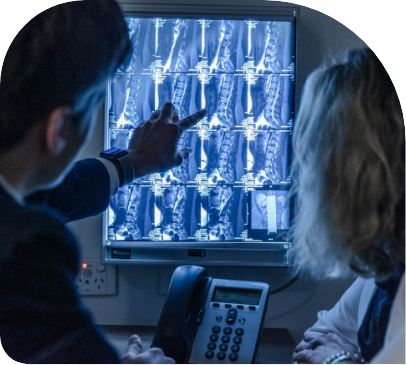
Post op imaging in the form of X rays and CT scans may be required during the hospital stay after surgery or at a later stage to confirm the integrity of the implants and shape of the spine. Fusion assessment with imaging is typically done in a delayed fashion as this takes 3 months or more for solid fusion to take place.
Possible complications of spinal instrumented procedures
The complication profile of instrumented spine surgery is similar to non-instrumented surgery in many regards (please refer to previous chapter). However, some possible complications are specific to instrumentation of the spine and/or inherent to the approach used to achieve it.
Some specific common complications related to anterior approaches to the spine include:
- Neck swelling with breathing difficulty caused by bleeding or blood clot formation in the neck – rare
- Hoarseness of voice – common
- Sore throat – common
- Damage to dura resulting in spinal fluid leakage – rare
- Paralysis is extremely rare but may be caused by a spinal cord injury
- Spinal nerve injury. Injury to these nerves is the most common reason for anterior cervical surgery and new nerve injuries can also occur
- Swallowing difficulties – common
- Others
- All of the serious risks listed above are quite rare and, in the majority of cases, transient.
- Injury to blood vessels causing significant bleeding
- Abdominal wall defects causing hernia
- Retrograde ejaculation in males
- Deep vein thrombosis (clot formation in deep veins)
- Abdominal pain and abdominal obstructions
- Lower limb weakness or numbness
- Abnormal warmth and swelling of leg caused by injury or bruising to the nerves controlling the size of the vessels in the leg
- Others
All the risks listed above are quite rare and, in the majority of cases, transient.
- Various hardware failures requiring revision surgery; examples include screw misplacement, screw loosening, breaking or pull out, cage migration, rod breaking, etc.
- Risk of neural injury during insertion of the implants; especially the screws.
- Risk of more surgeries down the line due to degeneration of the levels adjacent to the fused level(s).
- Failure of bone healing i.e., fusion to occur, may result in persistent or recurrent worsening of pain, or problems with instrumentation.
- Other unforeseen risks.

Recommendations for recovery at home
Recovery usually takes 4 to 6 weeks after uncomplicated spinal fusion. It may take longer in older patients and in case of severe pre-existing disability, or in cases where many spinal levels have been operated on.
- Avoid lifting heavy objects (more than 2kg).
- Bending and twisting movements should be minimized.
- Get advice from your physiotherapist on how to lift in case you have to.
- Driving is also usually not allowed for several weeks during recovery.
- Swimming and baths not allowed when the wound is not yet healed yet.
- Stay active: It is recommended to take regular walks and do daily light exercises to relieve back pain and hasten recovery. Sitting for long periods put the operated site at increased pressure.
- Take adequate rest: a good sleep helps the body to recovery faster. Patients may find their back is sore upon waking up, this usually settles after a short walk or a shower.
Return to work usually depends on how quickly the patient recovers, the level of symptoms and type of occupation.
Our surgical team will offer any more specific advice when need be.
