Hydrocephalus
What is hydrocephalus?
Hydrocephalus means “water on the brain”. The brain and spinal cord are surrounded by fluid, which provides support and protection, as well as removing waste molecules.
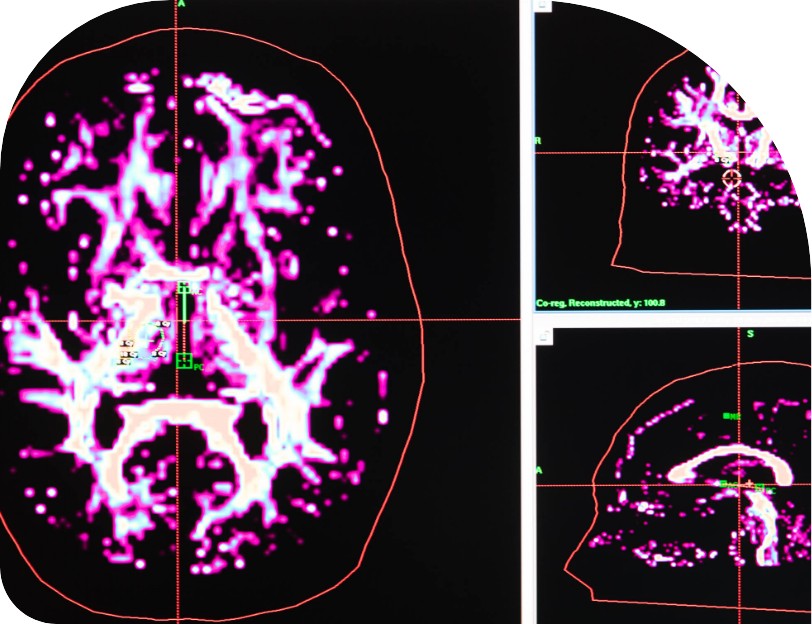
This “cerebrospinal fluid,” or CSF, is produced rapidly (around 20 mL every hour), circulates around the brain and spinal cord, and is then reabsorbed into the blood stream. Production and reabsorption of CSF must be exactly balanced; any slight difference will result in a build-up of CSF in the fluid spaces in the brain. This “water on the brain” is called hydrocephalus.
Why can hydrocephalus be dangerous?
The increased volume of fluid in the brain can be dangerous either by increasing the pressure inside the head, or by stretching the brain tissue causing it to malfunction.

What are the symptoms of hydrocephalus?
Hydrocephalus causing an increase in pressure generally causes headache, but can also damage vision and cause a loss of consciousness. Sometimes the pressure can build up without an obvious increase in CSF volume, as occurs with Benign Intracranial Hypertension (also called Idiopathic Intracranial Hypertension or Pseudotumour Cerebri).
In older patients, the increase in fluid volume may not cause an increase in pressure, but results in the characteristic presentation with urinary incontinence, difficulty walking, and short-term memory loss.
What can be the causes of hydrocephalus?
In very rare cases, the excess fluid results from an increase in fluid production, which is seen in certain tumours of the brain. Usually, the cause is obstruction of CSF circulation or impairment of CSF absorption back into the blood stream.
These conditions can result from tumours, head injury, bleeding into or around the brain, or blockage of the veins draining blood from the brain. Sometimes the cause is unknown.

How is hydrocephalus treated?
The best treatment for hydrocephalus is to treat the underlying cause. Unfortunately, this is usually not possible. Medications can be used to reduce the production of CSF (e.g. acetazolamide), but the usual treatment is to change the circulation of CSF.
In some cases, this is achieved by opening new pathways for CSF to leave the brain (endoscopic third ventriculostomy). In other cases, CSF is drained to other parts of the body to be reabsorbed, such as with a shunt from the brain to the abdomen (ventriculo-peritoneal shunt).
