Craniotomy
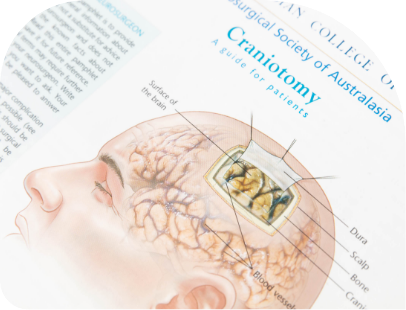
What is a Craniotomy?
A craniotomy is a surgical procedure aimed to create an opening in the skull (i.e., a bone flap).
This opening is performed to access the intracranial structures (e.g., the brain underneath) by means of specialised tools. Different types of craniotomies exist, according to the necessity. A craniotomy is performed to treat brain tumours, aneurysms or AVMs, traumatic head injury, hematomas (also called blood clots), infections, or to remove foreign bodies.

Reasons for the procedure
A craniotomy may be done for a variety of reasons, including, but not limited to:
- Performing a biopsy / resection of a brain / skull base tumour
- Clipping or repairing an aneurysm
- Removing blood or blood clots from a leaking blood vessel
- Removing an arteriovenous malformation (AVM) or addressing an arteriovenous fistula (AVF)
- Brain biopsy
- Draining a brain abscess
- Repairing a skull fracture
- Repairing a tear in the membrane lining the brain (dura mater)
- Relieving pressure in the brain after an injury or stroke
- Implanting stimulator devices (for example, for pain treatment or movement disorders such as Parkinson’s disease).
Before surgery
One of our specialists will explain the procedure, its risks and benefits, and there will be time to ask questions. Each patient is asked to sign a consent form and complete paperwork to inform the specialist about their medical history (e.g., allergies, medicines, previous surgeries). Presurgical tests (blood tests, electrocardiogram, chest X-ray) may be needed several days before surgery. A preoperative neurological examination will also be performed to obtain a neurological baseline and to compare it with the post-operative assessment.
Patients should inform their specialist if they:
- Are pregnant or think they may be
- Are sensitive to or allergic to any medicines, latex and/or anaesthetic agents, local or general
- Are taking certain medications (prescribed and over the counter) and/or herbal supplements
- Have a history of bleeding disorders or are taking any anticoagulant medicines (blood thinners such as aspirin, Plavix, Coumadin) that affect blood clotting. It may be necessary to stop these medicines a few days before surgery.
Smoking and drinking alcohol should be stopped as soon as possible before the procedure and a few weeks afterwards to avoid bleeding and healing problems.
Patients may be asked to wash their skin and hair with a special antiseptic soap and shampoo before surgery, in order to kill bacteria and reduce surgical site infections.
During surgery
A craniotomy can take one or many more hours, depending on the complexity of the procedure.
Generally, the procedure follows this process:
An intravenous (IV) line will be inserted in the patient’s arm or hand and a urinary catheter will be inserted to drain their urine. Patient will then lie on the operating table and be given general anaesthesia. The anaesthesiologist will continuously monitor the patient’s heart rate, blood pressure, breathing, and blood oxygen level.
The incision area of the scalp will be prepped with an antiseptic. There are various types of incisions that may be used, depending on the affected area of the brain. Incisions are usually made from behind the hairline in front of the ear and nape. A hair sparing technique is generally used, where only a 1/4-inch-wide area along the proposed incision is shaved.
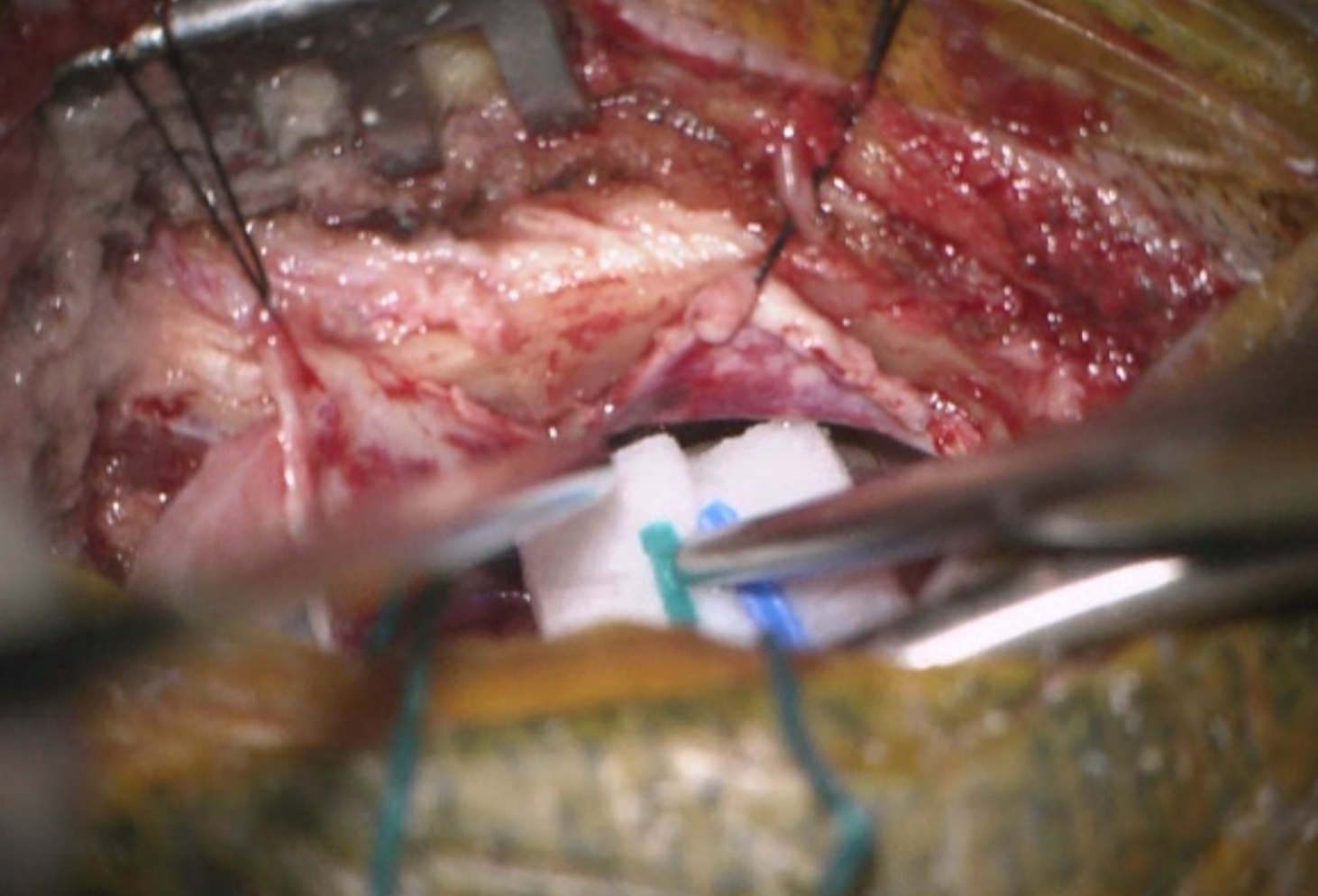
Patient’s head will be held in place by a device to be removed at the end of the procedure. The skin and muscles are pulled up and clipped to control bleeding while providing access to the brain. Small burr holes are then made in the skull with a medical drill. The cut bone flap is lifted and removed to expose the thick outer protective covering of the brain called the dura.
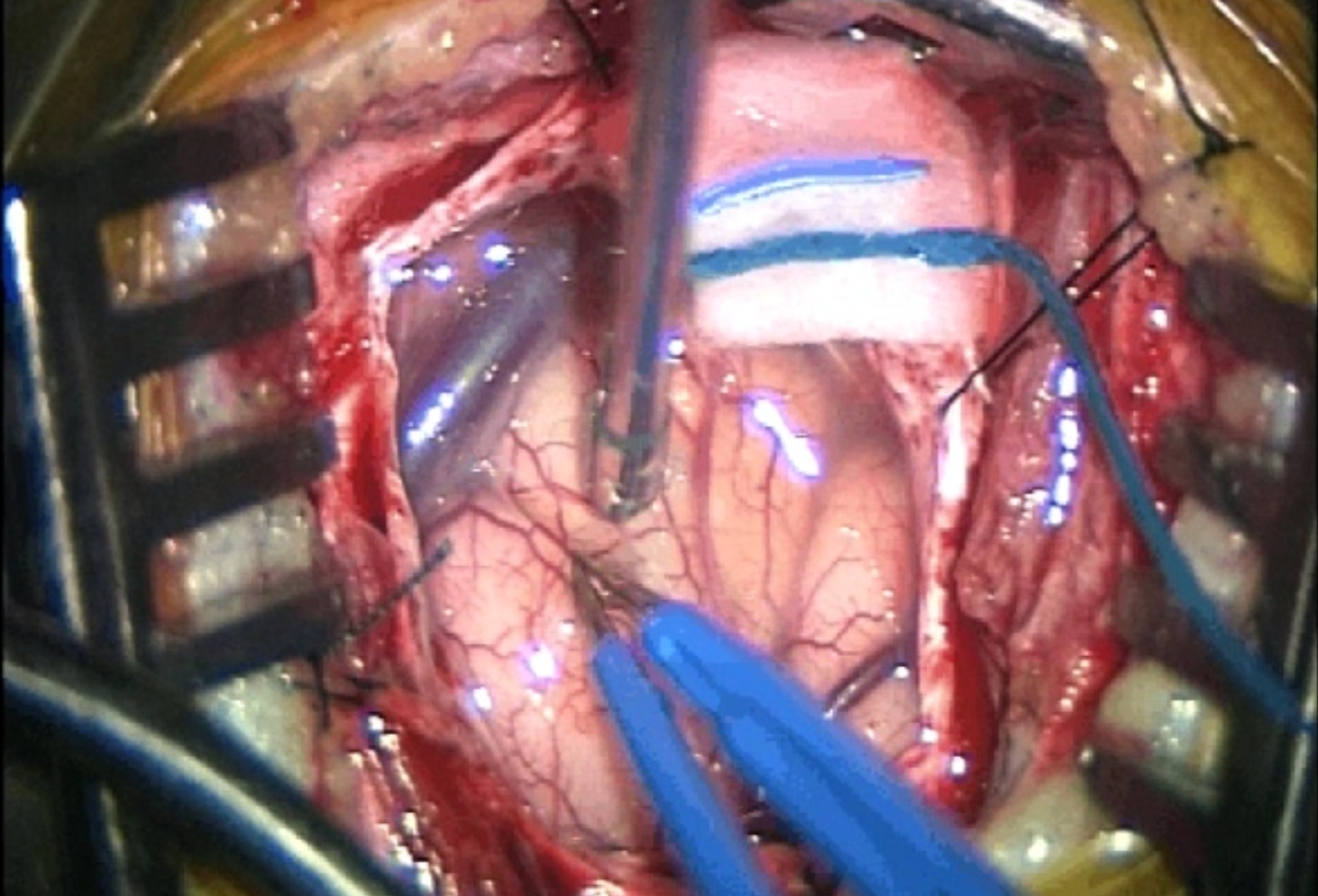
Once the dura is opened to expose the brain, excess fluid will be allowed to flow out of the brain, if need be. Microsurgical instruments, such as magnification glasses or an operating microscope, may be used by the surgeon to enable a better view of the brain structures.
The brain injury or disease is operated on – for example, ruptured blood vessels are repaired, or the blood clot or tumour is removed. Because the brain cannot be easily moved aside to access and fix problems, being enclosed inside the bony skull, neurosurgeons use a variety of very small instruments to work inside the brain (such as dissectors and medical drills, lasers, scissors).
Once the surgery is completed, any retractors are removed, and the dura is closed with sutures.
The bone flap is reattached in its original position and secured to the skull using plates and/or sutures, with or without meshes.
The plates and screws remain permanently to support the area, and they sometimes may be felt under the skin. A drain may be placed under the skin for a few days to remove blood or fluid from the area. The muscles and skin are sutured back together.
A sterile bandage or soft adhesive dressing is applied over the incision.
A craniotomy generally requires a hospital stay of 3 to 7 days. Patients may also go to a rehabilitation unit for several days after the hospital stay.
After surgery
Straight after the procedure, patient will be transferred to the recovery room to monitor their vital signs as they awake from anaesthesia. After they awaken, patients will be moved to the Intensive Care Unit (ICU) for close monitoring.
Each patient is asked to sign a consent form and complete paperwork to inform the specialist about their medical history (e.g., allergies, medicines, previous surgeries). Presurgical tests (blood tests, electrocardiogram, chest X-ray) may be needed several days before surgery. A preoperative neurological examination will also be performed to obtain a neurological baseline and to compare it with the post-operative assessment.

Patients may experience the following:
Nausea, headaches – symptoms that can be controlled by prescribed medications
Swollen and bruised eyes
Head may be elevated to about 30 degrees to reduce the risk of intracranial pressure
They will be frequently asked to move their arms, fingers, toes, and legs
Hospital staff will regularly test for any signs of brain damage – for instance, they may examine the patient’s pupils with a flashlight or ask simple questions
Steroid medication (to control brain swelling) and anticonvulsant medication (to prevent seizures) may be given depending on the type of brain surgery
Stitches or staples are usually removed about one week after surgery.
A post-operative appointment will be booked for each patient with the neurosurgeon in charge, 4 to 6 weeks after the surgery date.
Until then, follow the surgeon’s care instructions once back home. General suggestions include:
- No heavy lifting
- No strenuous activity including housework and contact sports
- No alcohol drinking, to avoid blood thinning and risk of bleeding, and no alcohol mixing with pain medicines
- No smoking or use of nicotine products such as vape. It may delay healing
- No driving, no flying, no return to work until the surgeon allows
- Gradual increase of the physical activity, starting with 5 to 10 minutes every 3 to 4 hours
- Keeping incision clean and dry: no bath, pool, or tub soaking. No lotion/ointment to be applied, including hair styling products
Should any help be required, our team of neurosurgeons at Macquarie Neurosurgery & Spine is available to answer all questions and discuss the patient’s recovery process.